Lumbar Spinal Stenosis
Almost everyone will experience low back pain at some point in their lives. A common cause of low back pain is lumbar spinal stenosis.
As we age, our spines change. These normal wear-and-tear effects of aging can lead to narrowing of the spinal canal. This condition is called spinal stenosis.
Anatomy
Understanding your spine and how it works can help you better understand spinal stenosis.
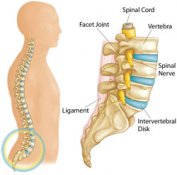
Your spine is made up of small bones, called vertebrae, which are stacked on top of one another. Muscles, ligaments, nerves, and intervertebral disks are additional parts of your spine.
Vertebrae
These bones connect to create a canal that protects the spinal cord. The spinal column is made up of three sections that create three natural curves in your back: the curves of the neck area (cervical), chest area (thoracic), and lower back (lumbar). The lower section of your spine (sacrum and coccyx) is made up of vertebrae that are fused together.
Five lumbar vertebrae connect the upper spine to the pelvis.
Parts Of The Lumbar Spine
Spinal Cord and Nerves
These “electrical cables” travel through the spinal canal carrying messages between your brain and muscles. Nerves branch out from the spinal cord through openings in the vertebrae.
Muscles and Ligaments
These provide support and stability for your spine and upper body. Strong ligaments connect your vertebrae and help keep the spinal column in position.
Facet Joints
Between vertebrae are small joints that help your spine move. Facet joints are very close to the spinal nerves.
Intervertebrae Disks
Intervertebral disks sit in between the vertebrae.
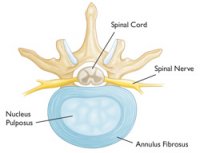
Healthy Intervertebral Disk (Cross-Sectional View)
When you walk or run, the disks act as shock absorbers and prevent the vertebrae from bumping against each other. They work with your facet joints to help your spine move, twist, and bend.
Intervertebral disks are flat and round, and about a half-inch thick. They are made up of two components.
Annulus fibrosus. This is the tough, flexible outer ring of the disk. It helps connect to the vertebrae.
Nucleus pulposus. This is the soft, jelly-like center of the annulus fibrosus. It gives the disk its shock-absorbing capabilities.
Description
Spinal stenosis occurs when the space around the spinal cord narrows. This puts pressure on the spinal cord and the spinal nerve roots, and may cause pain, numbness, or weakness in the legs.

As We Age, The Bone In Our Spines May Harden And Become Overgrown. This Can Lead To A Narrowing Of The Spinal Canal, Called Stenosis.
When stenosis occurs in the lower back. it is called lumbar spinal stenosis. It often results from the normal aging process. As people age, the soft tissues and bones in the spine may harden or become overgrown. These degenerative changes may narrow the space around the spinal cord and result in spinal stenosis.
Degenerative changes of the spine are seen in up to 95% of people by the age of 50. Spinal stenosis most often occurs in adults over 60 years old. Pressure on the spinal cord is equally common in men and women, athough women are more likely to have symptoms that require treatment.
A small number of people are born with back problems that develop into lumbar spinal stenosis. This is known as congenital spinal stenosis. It occurs most often in men. People usually first notice symptoms between the ages of 30 and 50.
Cause
Arthritis is the most common cause of spinal stenosis. Arthritis is the degeneration of any joint in the body.
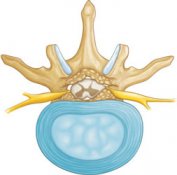
In the spine, arthritis can result as the disk degenerates and loses water content. In children and young adults, disks have high water content. As we get older, our disks begin to dry out and weaken. This problem causes settling, or collapse, of the disk spaces and loss of disk space height.

When We Are Young, Disks Have A High Water Content (Left). As Disks Age And Dry Out, They May Lose Height Or Collapse (Right). This Puts Pressure On The Facet Joints And May Result In Arthritis.
As the spine settles, two things occur. First, weight is transferred to the facet joints behind tghe spinal cord. Second, the tunnels that the nerves exit through become smaller.
As the facet joints experience increased pressure, they also begin to degenerate and develop arthritis and can hypertrophy (enlarge). The cartilage that occurs and protects the joints wears away. If the cartilage wears away completely, it can result in bone rubbing on bone. To make up for the lost cartilage, your body may respond by growing new bone in your facet joints to help support the vertebrae. Over time, this bone overgrowth-called spurs-may narrow the space for the nerves to pass through.
Degenerative Bone Spurs Narrow The Spinal Canal
Another response to degeneration in the lower back is that ligaments around the spine like the ligamentum flavum (yellow ligament) increase in size. This also lessens space for the nerves. Once the space has become small enough to irritate spinal nerves, painful symptoms result. Severe stenosis can cause weakness and even paralysis in the legs and difficulty with bladder and bowel function.
Symptoms
Back Pain. People with spinal stenosis may or may not have back pain, depending on the degree of degeneration that has developed.

Spinal Nerves Relay Sensation In Specific Parts Of Your Body. Pressure On The Nerves Can Cause Pain In The Areas That The Nerves Supply. Pain In The Buttocks That Radiates Down The Leg – Called Sciatica – Is Caused By This Pressure.
Burning pain in buttocks or legs (sciatica). Pressure on spinal nerves caaresult i pain in the areas that the nerves supply. The pain may be described as an ache or a burning feeling. It typically starts in the area of the buttocks and radiates down the legs. The pain down the leg is often called “sciatica”. As it progesses, iit can result in pain in the foot.
Numbness or tingling in buttocks or legs. As pressure in the nerve increases, numbness and tingling often accompany the burning pain. Although not all patients will have both burning pain and numbness and tingling.
Weakness in the legs or “foot drop”. Once the pressure reaches a critical level, weakness can occur in one or both legs. Some patients will have a foot-drop, or the feeling that their foot slaps on the ground while walking.
Less pain with leaning forward or sitting. Studies of the lumbar spine show that leaning forward can actually increase the space available for the nerves. Many patients may note relief when leaning forward and especially with sitting. Pain is usualy made worse by standing up straight and walking. Some patients note that they can ride a stationary bike or walk leaning on a shopping cart. Walking more than 1 or 2 blocks, however, may bring on severe sciatica or weakness. This is called pseudo-claudication.
Doctor Examination
Medical History and Physical Examination
After discussing your symtoms and medical history, your doctor will examine your back. This will include looking at your back and pushing on different areas to see if it hurts. Your doctor may have you bend forward, backward, and side-to-side to look for limitations or pain.
Imaging Tests
Other tests which may help your doctor confirm your diagnosis include:
X-rays. Although they only visualize bones, X-rays can help determine if you have spinal stenosis. X-rays will show aging changes, like loss of disk height or bone spurs.
X-rays taken while you lean forward and backward can show “instability” in your joints. X-rays can also show too much mobility. This is called spondylolisthesis.
Magnetic resonance imaging (MRI). This study can create better images of soft tissues, such as muscles, disks, nerves, and the spinal cord.
Additional tests. Computed tomography (CT) scans can create cross-section images of your spine.
Treatment
Nonsurgical Treatment
Nonsurgical treatment options focus on restoring function and relieving pain. Although nonsurgical methods do not improve the narrowing of the spinal canal, many people report that these treatments do help relieve symptoms for a while.
Physical therapy. Stretching exercises, massage, and lumbar and abdominal strengthening often help manage symptoms.
Lumbar traction. Although it may be helpful in some patients, traction has very limited results. There is no scientific evidence of its effectiveness.
Anti-inflammatory medications. Because stenosis pain is caused by pressure on spinal nerves, reducing inflammation (swelling) around the nerve may relieve pain. Non-steroidal anti-inflammatory drugs (NSAIDs) initially provide pain relief. When used over the course of 5-10 days, they can also have an anti-inflammatory effect. However long term use of NSAIDs and even stronger narcotics is not advisable. The pain may be relieved but the stenosis and nerve pressure remains.
Most people are familiar with nonprescription NSAIDs, such as aspirin and ibuprofen. Whether over-the-counter or prescription strength, these medicines must be used carefully. They can lead to gastritis or stomach ulcers. If you develop acid reflux or stomach pains while taking an anti-inflammatory,be sure to talk with your doctor.
Steriod injections. Cortisone is a powerful anti-inflammatory. Cortisone injections around the nerves or in the “ëpidural space” can decrease swelling, as well as pain. It is not recommended to receive these, however, more than 3 times. These injections are more likely to decrease pain and numbness but not weakness of the legs. Again they do not take away nerve pressure that can cause weakness and paralysis.
Chiropractic manipulation. Care should be taken if a patient has osteoporosis or disk herniation. Manipulation of the spine in these cases can worsen symptoms or cause other injuries.
Surgical Treatment
Surgery for lumbar spinal stenosis is generally reserved for patients who have poor quality of life due to pain and weakness. Patients may complain of inability to walk for an extended length of time without sitting. This is often the reason that patients consider surgery.
There are several surgical options to treat lumbar spinal stenosis: Microsurgical decompression with or without laminectomy, spinal fusion, and posterior dynamic stabilization without fusion. Modern options can result in excellent pain relief. Be sure to discuss the advantages and disadvantages of different surgeries with your doctor.
Laminectomy. This procedure involves removing the bone, bone spurs, and ligaments that are compressing the nerves. This procedure may also be called a “decompression”. Laminectomy can be performed as open surgery, where your doctor uses a single, larger incision to access your spine. The procedure can also be done using a minimally invasive method, where several smaller incisions are made. Your doctor will discuss with you the right option for you.
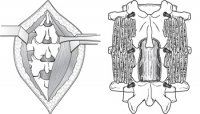
(Left) To Access The Spine, Muscles Are Pulled Back To Expose The Bone. (Right) After The Laminectomy, Bone Graft Material And Screws Are Placed Along The Sides Of The Vertebrae To Help With Healing.
Spinal fusion. If spinal degeneration has progressed to spinal instability, a combination of microsurgical decompression and stabilization or spinal fusion may be recommended.
In a spinal fusion, two or more vertebrae are permanently healed or fused together. A bone graft taken from the pelvis or hip bone is used to fuse the vertebrae. More options include use of a ceramic cage between the vertebrae with bone promoting material in or around the cage. BMP may be used to aid fusion. Fusion eliminates motion between vertebrae and prevents the slippage from worsening after surgery. The surgeon may also use rods and screws to hold the spine in place while the bones fuse together. The use of rods and screws makes the fusion of the bones happen faster and speeds recovery.
Posterior Dynamic Stabilization
This is a modern method to stabilize the spine without fusion and is usually used after microsurgical decompression.
Rehabilitation. After surgery, you may stay in the hospital for a short time, depending on your health and the procedure performed. Healthy patients who undergo just decompression may go home the same or next day, and may return to normal activities after only a few weeks. Fusion generally adds 2 to 3 days to the hospital stay.
Your surgeon may give you a brace or corset to wear for comfort. He or she will likely encourage you to begin walking as soon as possible. Most patients do not need physical therapy except to learn how to strengthen their backs.
Your physical therapist may show you exercises to help you build and maintain strength, endurance, and flexibility for spinal stability. Some of these exercises will h elp strengthen your abdominal muscles, which help support your back. Your physical therapist will create an individualized program, taking into consideration your health and history.
Most people can go back to a desk stop within a few days to a few weeks after surgery. They may return to normal activities after 2 to 3 months. Older patients who need more care and assistance may be transferred from the hospital to a rehabilitation facility prior to going home.
Surgical risks. There are minor risks associated with every surgical procedure. These include bleeding, infection, blood clots, and reaction to anesthesia. These fisks are usually very low.
Elderly patients have higher rates of complications from surgery. So do overweight patients, diabetics, smokers, and patients with multiple medical problems.
Specific complications from surgery for spinal stenosis include:
- Tear of the sac covering the nerves (dural tear)
- Failure of the bone fusion to heal
- Failure of screws or rods
- Nerve injury
- Need for further surgery
- Failure to relieve symptoms
- Returen of symptoms
Surgical outcomes. Overall, the results of laminectomy with or without spinal fusion for lumbar stenosis are good to excellent in approximately 80% of patients. Patients need to see more improvement of leg pain than back pain. Most patients are able to resume a normal lifestyle after a period of recovery from surgery.
New Surgical Options
Interspinous Process Devices
Interspinous process devices have been developed as a minimally invasive surgical option for lumbar spinal stenosis. A spacer fits between the spinous processes in the back of the spine. Its role is to keep the space for the nerves open by spreading the vertebrae apart.
Interspinous process spacers were approved in 2005. Many procedures have been performed since then. In some studies, success rates are greater than 80 percent.
Numerous spacer devices are currently being evaluated. They may be a safe alternative to an open laminectomy for some patients. Limited bone (lamina) is removed with this procedure, and it may be performed under local anesthesia.
The key to success with this procedure is appropriate selection of the patients. The appropriate candidate must have relief of buttock and leg pain when sitting or bending forward. The pain returns upon standing.
Minimally Invasive Decompression
Decompression can be performed using smaller incisions. Recovery is often quicker with minimally invasive techniques. This is because there is less injury to the surrounding soft tissues.
With these minimally invasive techniques, surgeons rely more on microscopes to see the area for surgery. They may also take X-rays during the operation. A traditional open procedure requires more direct visualization of the patient’s anatomy, and therefore requires a larger incision. This can be more painful for the patient.
The limitation of minimally invasive surgery is the degree of visualization available. If the spinal stenosis extends over a large area of the spine, an open technique is the only method that can address the problem.
The advantages of minimally invasive procedures include reduced hospital stays and recovery periods. However, both open and minimally invasive techniques relieve stenosis symptoms equally. Your doctor will be able to discuss with you the options that best meet your healthcare needs.










